Prescription for a Stress-Free Payday
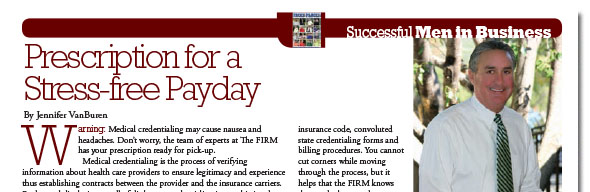
By Jennifer Van Bueren
“Warning: Medical credentialing may cause nausea and headaches. Don’t worry, the team of experts at The FIRM has your prescription ready for pick-up. Medical credentialing is the process of verifying information about health care providers to ensure legitimacy and experience thus establishing contracts between the provider and the insurance carriers. Far beyond displaying a wall of diplomas, credentialing is a multi-tiered process that requires careful and thorough recording, tracking and followthrough. Since patients who pay out of pocket are few and far between,
proper credentialing ensures that physicians can accept third party reimbursement from private insurance companies, Medicare and Medicaid.”