California Medical Association News – Coding Corner: Modifier 59 -May 01, 2018 |
Practice Management
CPR’s “Coding Corner” focuses on coding, compliance, and documentation issues relating specifically to physician billing. This month’s tip comes from G. John Verhovshek, the managing editor for AAPC, a training and credentialing association for the business side of health care.
Modifier 59 Distinct procedural service is an “unbundling modifier.” When properly applied, it allows you to separately report—and to be reimbursed for—two or more procedures that normally would not be billed or paid independently during the same provider/patient encounter. For example, per CPT Assistant (Jan. 2018):
Code 20680 [Removal of implant; deep (eg, buried wire, pin, screw, metal band, nail, rod or plate)] describes a unit of service that is typically reported only once, provided the original injury is located at only one anatomic site, regardless of the number of screws, plates, or rods inserted, or the number of incisions required for removal. The removal of a single implant system or construct, which may require multiple incisions (eg, intramedullary [IM] nail and several locking screws) is reported only once with code 20680.
Reporting code 20680 more than once is appropriate only when the hardware removal is performed for another fracture(s) in a different anatomical site(s) unrelated to the first fracture (eg, ankle hardware and wrist hardware). In these circumstances, modifier 59, Distinct Procedural Service, would be appended to subsequent uses of the implant removal code.
CPT® and CCI Conditions to Append Modifier 59
As outlined in the CPT® codebook, the general conditions under which you might append modifier 59 include situations where two or more CPT® codes, not normally reported together, are performed at a:
Different session
Different procedure or surgery
Different site or organ system:
This condition “does not include treatment of contiguous structures of the same organ,” according to national Correct Coding Initiative (CCI) Chapter 1 guidelines, which apply to all Medicare payers. “For example, treatment of the nail, nail bed, and adjacent soft tissue constitutes treatment of a single anatomic site. Treatment of posterior segment structures in the ipsilateral eye constitutes treatment of a single anatomic site. Arthroscopic treatment of a shoulder injury in adjoining areas of the ipsilateral shoulder constitutes treatment of a single anatomic site.”
Separate incision/excision
Separate lesion or separate injury: Chapter 1 CCI guidelines clarify, “Use of modifier 59 to indicate different procedures/surgeries does not require a different diagnosis for each HCPCS/CPT coded procedure/surgery. Additionally, different diagnoses are not adequate criteria for use of modifier 59. The HCPCS/CPT codes remain bundled unless the procedures/surgeries are performed at different anatomic sites or separate patient encounters.”
Guidelines provide examples of proper use
Modifier 59 is necessary only if you wish to report/bill two services that normally are bundled. For Medicare and any payer that follows Centers for Medicare & Medicaid Services (CMS) guidelines, the surest way to confirm if two codes are bundled is to consult CCI edits. Any two codes designated within the CCI as “mutually exclusive,” or that are paired together as “column 1” and “column 2” codes, are bundled and not typically reported separately. Each CCI code pair edit includes a correct coding modifier indicator of “0” or “1.” A “0” indicator means that you may not unbundle the edit combination, under any circumstances. An indicator of “1” means that you may use a modifier (such as modifier 59) to override the edit, if the procedures are distinct from one another.
CCI Chapter 1 guidelines specify three conditions under which modifier 59 will always apply:
When a diagnostic procedure precedes a surgical or non-surgical therapeutic procedure and is the basis on which the decision to perform the surgical or non-surgical therapeutic procedure is made, that diagnostic procedure may be considered to be a separate and distinct procedure as long as: (a) it occurs before the therapeutic procedure and is not interspersed with services that are required for the therapeutic intervention; (b) it clearly provides the information needed to decide whether to proceed with the therapeutic procedure; and (c) it does not constitute a service that would have otherwise been required during the therapeutic intervention. If the diagnostic procedure is an inherent component of the surgical or non-surgical therapeutic procedure, it shall not be reported separately.
When a diagnostic procedure follows a surgical procedure or non-surgical therapeutic procedure, that diagnostic procedure may be considered to be a separate and distinct procedure as long as: (a) it occurs after the completion of the therapeutic procedure and is not interspersed with or otherwise commingled with services that are only required for the therapeutic intervention; and (b) it does not constitute a service that would have otherwise been required during the therapeutic intervention. If the post-procedure diagnostic procedure is an inherent component or otherwise included (or not separately payable) post- procedure service of the surgical procedure or non-surgical therapeutic procedure, it shall not be reported separately.
There is an appropriate use for modifier 59 that is applicable only to codes for which the unit of service is a measure of time (e.g., per 15 minutes, per hour). If two separate and distinct timed services are provided in separate and distinct time blocks, modifier 59 may be used to identify the services. The separate and distinct time blocks for the two services may be sequential to one another or split. When the two services are split, the time block for one service may be followed by a time block for the second service, followed by another time block for the first service. All Medicare rules for reporting timed services are applicable. For example, the total time is calculated for all related timed services performed. The number of reportable units of service is based on the total time, and these units of service are allocated between the HCPCS/CPT codes for the individual services performed. The physician is not permitted to perform multiple services, each for the minimal reportable time, and report each of these as separate units of service. (e.g., A physician or therapist performs eight minutes of neuromuscular reeducation (CPT code 97112) and eight minutes of therapeutic exercises (CPT code 97110). Since the physician or therapist performed 16 minutes of related timed services, only one unit of service may be reported for one, not each, of these codes.)
When appending modifier 59 to break a CCI edit, you should always append the modifier to the secondary (“column 2”) code. The CCI guidelines provide two examples to illustrate proper application of modifier 59:
Example #1: The column one/column two code edit with column one CPT code 38221 (Diagnostic bone marrow biopsy) and column two CPT code 38220 (Diagnostic bone marrow, aspiration) includes two distinct procedures when performed at separate anatomic sites (e.g., contralateral iliac bones) or separate patient encounters. In these circumstances, it would be acceptable to use modifier 59. However, if both 38221 and 38220 are performed on the same iliac bone at the same patient encounter which is the usual practice, modifier 59 shall NOT be used. Although CMS does not allow separate payment for CPT code 38220 with CPT code 38221 when bone marrow aspiration and biopsy are performed on the same iliac bone at a single patient encounter, a physician may report CPT code 38222 (Diagnostic bone marrow; biopsy(ies) and aspiration(s)).
Example #2: The procedure to procedure edit with column one CPT code 11055 (Paring or cutting of benign hyperkeratotic lesion …) and column two CPT code 11720 (Debridement of nail(s) by any method; 1 to 5) may be bypassed with modifier 59 only if the paring/cutting of a benign hyperkeratotic lesion is performed on a different digit (e.g., toe) than one that has nail debridement. Modifier 59 shall not be used to bypass the edit if the two procedures are performed on the same digit.
Modifier 59 should be your last resort
You should append modifier 59 only if no other modifier applies. CCI guidelines confirms this: “Modifier 59 shall only be used if no other modifier more appropriately describes the relationships of the two or more procedure codes.”
For example, guidelines in the microbiology subsection of the CPT® codebook illustrate when modifier 91 Repeat clinical diagnostic laboratory test is preferable to modifier 59 when reporting repeat laboratory tests performed on the same day:
Presumptive identification of microorganisms is defined as identification by colony morphology, growth on selective media, Gram stains, or up to three tests (eg, catalase, oxidase, indole, urease). Definitive identification of microorganisms is defined as an identification to the genus or species level that requires additional tests (eg, biochemical panels, slide cultures). If additional studies involve molecular probes, chromatography, or immunologic techniques, these should be separately coded in addition to definitive identification codes (87140-87158). For multiple specimens/sites use modifier -59. For repeat laboratory tests performed on the same day, use modifier -91.
Finally, you should never append modifier 59 to evaluation and management (E/M) service codes (e.g., outpatient office visits 99201-99215). For example, to report an E/M service that results in the decision to perform a major surgical procedure (i.e., a procedure with a 90-day global period), and that E/M service occurs on either the day of, or the day before, a major surgical procedure, you should report the appropriate E/M code with modifier 57 Decision for surgery appended. For a separate E/M service that determines the need for a minor procedure (i.e., any procedure with a global period of less than 90 days), you should turn to modifier 25 Significant, separately identifiable evaluation and management (E/M) service by the same physician on the day of a procedure.
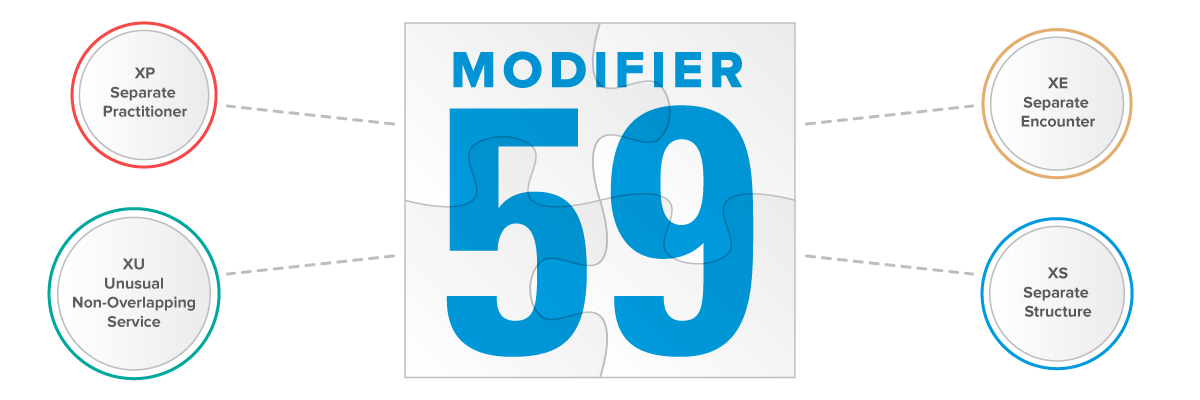
X{EPSU} modifiers provide an alternative to 59
Effective for dates of service beginning January 1, 2015, CMS released four new modifiers for Medicare claims, to be appended in lieu of 59 Distinct procedural service under defined circumstances. CMS describes the new modifiers, announced in CMS Transmittal 1422, Change Request 8863, as “subsets of distinct procedural services (-59 modifier),” to include:
XE – Separate Encounter – Used to describe services that are separate because they take place during separate encounters;
XS – Separate Structure – Used to describe services that are separate because they are performed on different anatomic organs, structures or sites;
XP – Separate Practitioner – Used to describe services that are distinct because they are performed by different practitioners; and
XU – Unusual Non-Overlapping Service – Used to describe services that are distinct because they do not overlap the usual components of the main service.
Currently, use of the X{EPSU} modifiers is not mandatory; however, CMS has encouraged immediate adoption of the X{EPSU} modifiers by all Medicare payors, stating, “contractors are not prohibited from requiring the use of selective modifiers in lieu of the general -59 modifier when necessitated by local program integrity and compliance needs.” As such, not only should medical providers prepare for the new modifiers, they should also expect even greater scrutiny of any modifier 59 claims, as well.
Questions about Medical Coding, Modifier, codes and reimbursement? Physician Credentialing and Revalidation ? or other changes in Medicare, Commercial Insurance, and Medicaid billing, credentialing and payments? Call the Firm Services at 512-243-6844