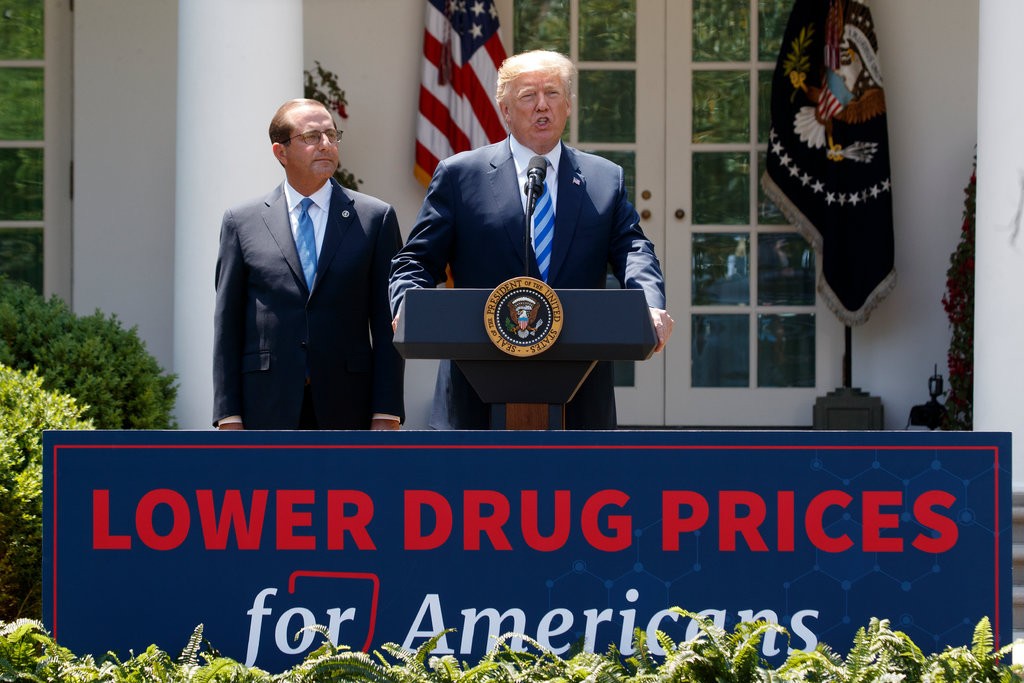
Trump administration proposes new Medicare drug payment model to reduce costs
HEALTHCARE FINANCE- Susan Morse, Senior Editor October 25,2018 The International Pricing Index model would reset Medicare payments for physician-administered drugs. President Trump on Thursday proposed to reduce prescription drug costs in…