Healthcare Dive- Meg Bryant- June 13, 2018
The push toward valued-based care and population health management has raised visibility around nonmedical conditions that impact health outcomes.
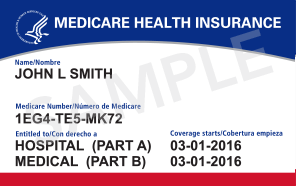
Improving health outcomes using population health strategies could get a major boost with a new Medicare Advantage rule taking effect this week.
Payers will now be able to work with companies like Uber or Lyft to provide transportation, for example, as part of a more complete set of benefits for the quickly growing MA population.
CMS issued a final rule in May giving MA plans more flexibility in determining the types of supplemental benefits they can offer chronically ill enrollees, including nonmedical benefits. The new policy, part of a broad 2019 Medicare payment rule, means plans like UnitedHealthcare and Humana aren’t harnessed to a set palette of supplemental benefits for members with chronic conditions, but can tailor them to the specific needs of individuals.
Providers have praised the expansion of benefits. “We now have a funding stream effectively within Medicare Advantage around social services,” Don Crane, president and CEO of America’s Physician Groups (APG), told Healthcare Dive in an interview. He called the change a “necessary and appropriate step” in managing chronic diseases.
The focus on social determinants of health and population health management is part of the broader shift to value-based care and reimbursement. Some providers, payers and employers already offer wellness and prevention programs or free rides to cut down on patient no-shows.
Whether the CMS rule leads to wider adoption of population health programs generally remains to be seen, but as a fast-growing segment of the Medicare market, insurers and providers are likely to be watching for any impact on access to care, outcomes and cost.
Currently, about 21 million Americans are enrolled in MA plans — or a little more than a third of Medicare beneficiaries. However, L.E.K Consulting predicts enrollment will jump to 38 million, or 50% of market penetration, by 2025.
‘Reasonable expectation of improving health’
Under the bipartisan budget deal signed by the president in February, Congress expanded supplemental benefits for the chronically ill to include ones that “have a reasonable expectation of improving or maintaining the health or overall function of the chronically ill enrollee and may not be limited to being primarily health related benefits.” The law also authorizes CMS to waive uniformity requirements, but only with respect to supplemental benefits for enrollees with chronic conditions.
Uber and Lyft, both with active partnerships in healthcare, say the new policy will help them expand their footprint.
Questions about ACA, private Medical Insurance and health insurance reimbursement? Physician Credentialing and Revalidation ? or other changes in Medicare, Commercial Insurance, and Medicaid billing, credentialing and payments? Call the Firm Services at 512-243-6844